Laura was 29 and seemed to have it all—a prestigious degree, a coveted job, and the praise of her colleagues. Yet, her regular alcohol abuse, normalized by a high-achieving but high-pressure environment, clouded her judgment. She didn’t see her drinking as a problem; her life was still on an upward trajectory—or so it seemed.
Her distance from friends and family was the first red flag that Laura’s lifestyle was not as sustainable as she believed. The high-stress nature of her job only fueled her reliance on alcohol, leading her to a critical crossroads. Her family watched with concern, knowing the path she was on could only lead to hardship and suffering. But Laura’s story doesn’t end there. And this is not a pitch for the rehab center that became her turning point.
Laura’s competitive spirit, the very trait that propelled her to academic and professional success, also sparked her commitment to recovery. Recognizing her substance abuse and rigid mindset as barriers to progress, she embarked on a journey to reclaim her health and well-being.
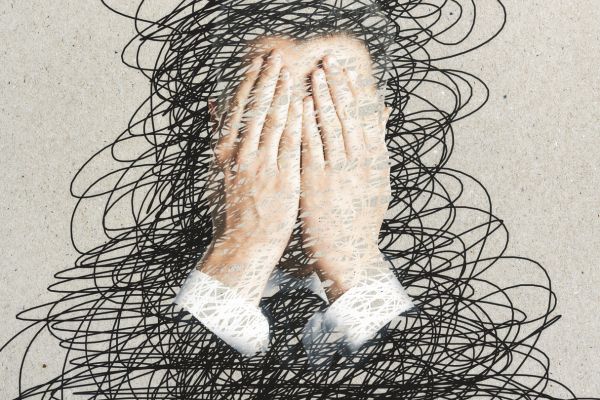
Understanding Hesitation: Common Barriers to Committing to Rehab
It’s not unusual to feel hesitant about seeking help for substance abuse. Understanding these common barriers can help you, or someone you care about, to move past them:
Fear of Judgment or Stigma
The fear of being judged for struggling with addiction is a common concern for many. Yet, as society’s understanding deepens, compassion is increasingly the response to those seeking treatment. It’s essential to recognize the importance of putting your health and well-being above societal opinions.
This realization is often challenging, particularly if your social circle has been a central part of your life. There might be a fear that stepping away from rehab could be seen as abandoning your friends. However, true friends will understand and support your journey towards betterment. Surrounding yourself with people who encourage your recovery is crucial. Anyone who views your decision to enter rehab as abandonment may not have your best interests at heart.
Concerns About Privacy
Privacy and confidentiality are foundational pillars of alcohol rehabilitation programs. When you commit to a rehab program, you can trust that your personal information, treatment details, and any disclosures made during therapy are safeguarded with the utmost discretion.
These programs are bound by strict privacy laws, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, which ensure that your journey to recovery remains a private affair between you and your healthcare providers. This commitment to confidentiality is designed to create a safe and secure environment where you can focus on your healing without the concern of external judgment or unwarranted disclosure.
The Cost of Treatment
Alcohol rehab can fit various budgets with insurance coverage, sliding scale fees based on income, and potential financing plans. Explore grants and government aid if uninsured. Treatment centers aim to make recovery financially attainable, so don’t hesitate to discuss your situation with them.
Fear of Failure
Fear of failure in alcohol rehab is natural, but remember, most who commit to a program see reduced relapse rates and sustained sobriety. Success rates are encouraging, and rehab doesn’t end at discharge—aftercare and alums support continue to back your recovery journey. You’re not alone; rehab equips you with the tools for success.
Uncertainty About Life Post-Rehab
Aftercare bridges the gap between rehab and everyday life, ensuring long-term success. Rehab centers lay the groundwork for seamless reintegration by providing ongoing support, resources, and counseling. They equip individuals with coping strategies, relapse prevention plans, and a supportive community to lean on. This continuous support helps individuals navigate the complexities of ‘normal’ life post-rehab, promoting sustained sobriety and well-being. Establishing a post-rehab exercise routine can also do wonders for cementing your recovery into lasting change that sticks.
Misconceptions About Rehab
Rehabilitation can be such a beneficial period, but it is often shrouded in misconceptions. In reality, it’s a structured environment that offers evidence-based treatments tailored to individual needs. Beyond the stereotypical group sessions, rehab provides a blend of therapy options, including cognitive-behavioral therapy, medication-assisted treatments, and holistic approaches like mindfulness and fitness programs. Each plan is designed to address the root causes of addiction, facilitate healing, and develop healthier coping mechanisms, all within a safe and supportive setting that respects the individual’s pace and privacy.
Denial or Underestimation of Addiction
Recognizing addiction starts with honest self-reflection on how substance use affects daily life. Signs include increased tolerance, withdrawal symptoms, neglecting responsibilities, and continued use despite negative consequences. Understanding the severity involves acknowledging the physical, emotional, and social toll of addiction. When substance use becomes a central focus, interfering with work, relationships, and health, it’s a clear indicator that professional help is needed. Accepting this reality is the first critical step towards seeking rehabilitation and reclaiming control over one’s life.
Worry About Work and Family Responsibilities
Balancing treatment with work and family commitments is manageable through careful planning and understanding your legal rights. Many rehab centers offer flexible programs, such as evening outpatient services, to accommodate work schedules. For family obligations, planning with relatives or utilizing community resources for childcare can provide support. Legally, the Family and Medical Leave Act (FMLA) in the United States allows eligible employees to take unpaid, job-protected leave for medical reasons, including substance abuse rehabilitation, ensuring they can prioritize their health without risking their employment. It’s important to communicate with your employer and explore the protections and options available for taking the necessary time for recovery.
Fear of the Unknown
A typical day in rehab is structured to provide stability and focus on recovery. You’d start with a healthy breakfast followed by a morning therapy session, such as cognitive-behavioral therapy or group counseling, to address mental health and addiction issues. Post-lunch activities often include skill-building workshops or fitness activities, fostering psychological and physical well-being.
The afternoons might be for individual therapy or specialized sessions, such as stress management. Evenings usually wind down with peer support groups like AA meetings, providing a sense of community and shared experience. Throughout the day, there are breaks for reflection, journaling, or relaxation, ensuring a balanced approach to recovery. This is, of course, a general framework, and the average day at rehab can vary across different facilities.
Taking Action: Next Steps to Overcome Barriers To Entering Rehab
Encourage readers to take proactive steps to overcome these barriers, such as:
- Reaching out to a trusted friend or family member to discuss their concerns.
- Scheduling a confidential consultation with a rehab facility to ask questions.
- Attending a local support group meeting to hear from others who have been through the process.
- Write down a list of pros and cons to visualize the benefits of seeking treatment.
Assessing Personal Requirements for Effective Alcohol Rehab Selection
If you or a loved one is facing a similar battle with addiction, it is crucial to choose a drug or alcohol rehabilitation center that aligns with your unique needs. Here is how to start:
1. Define Your Needs and Goals:
Understanding the specific challenges you face is the first step towards recovery. Whether it’s the nature of your addiction or co-occurring mental health conditions, clarifying your goals is essential.
2. Research Options:
Begin with a simple Google search, explore maps for proximity, and consult online directories to find centers that cater to your criteria.
3. Evaluate Treatment Programs:
From inpatient to outpatient and partial hospitalization, identify the program structure that best fits your lifestyle and recovery needs.
4. Check Credentials:
Ensure your chosen facility is not only licensed but also accredited, confirming their adherence to high care standards.
5. Understand Your Coverage:
Financial considerations are crucial. Determine how your insurance aligns with potential rehab centers and what out-of-pocket expenses you might expect.
6. Inquire and Interact:
Reach out with questions about staff credentials, treatment success rates, and the inclusion of family in the recovery process.
By taking these informed steps, you can navigate toward a rehab center that supports your journey to a healthier life.
Find an Alcohol Rehab Center Near You Today
Laura’s success story began with a simple online search by typing in alcohol rehab near me—a search that led her to share her experience and advocate for the life-changing benefits of a credible rehabilitation program.
Remember, struggling with addiction does not reflect on your character. It’s an intricate issue, often tied to deeply rooted behaviors and patterns that can be difficult to break free from. However, the decision to step back and assess your life objectively is a decisive move toward empowerment and healing.
Taking that first step, much like Laura took, is an act of bravery. It’s a recognition that while your journey is uniquely yours, you don’t have to walk it alone.
Take the First Step Towards Your New Horizon
Every journey begins with a single step—a step toward healing, understanding, and a healthier future. If Laura’s story resonates with you, or if you recognize the need for change in your own life or that of a loved one, we invite you to reach out.
Don’t let uncertainty hold you back. Contacting a rehab center or just having a conversation can be the most critical move toward recovery you’ll ever make. You’re not committing to anything by picking up the phone or sending an email—you’re just gathering information to make the best decision for you.
So, take that step. Reach out to a rehab center, consult with a healthcare professional, or simply talk to someone you trust about your options. Your path to recovery is waiting, and it starts with you making the brave decision to seek help. It’s not just about overcoming addiction; it’s about reclaiming your life.
Start Your Journey to a Better Tomorrow – Find an Alcohol Rehab facility near your zip code today.